For many people, identifying their personal battle with substance abuse is the first step toward recovery. The following step is to locate a therapy program that can assist them in regaining their total health, well-being, and happiness.

A person can choose from an infinite number of therapy alternatives. For instance, some individuals suffering from severe forms of addiction may enroll in a detox program prior to entering treatment. Others may elect to begin their recovery in an inpatient or outpatient setting. Following treatment, it is important to reinforce the principles learnt during recovery by participating in support groups and therapy sessions.
It is not simple to recover from addiction. To attain and sustain long-term sobriety will require a great degree of effort and self-discipline. On this trip, you will never be alone. You’ll develop close bonds with other people in recovery who understand what you’re going through during rehabilitation. During this difficult time, your family, friends, and other loved ones are also looking out for your best interests.
Your success in recovering from addiction is directly related to your commitment to the process. Learn about the many treatment options for addiction below to gain a better understanding of what lies ahead.
Types of Addiction Treatment Services
Treatment regimens are unique to each individual and can be tailored to their specific requirements and circumstances. The most effective treatment programs involve persons in recovery in every step of the process.
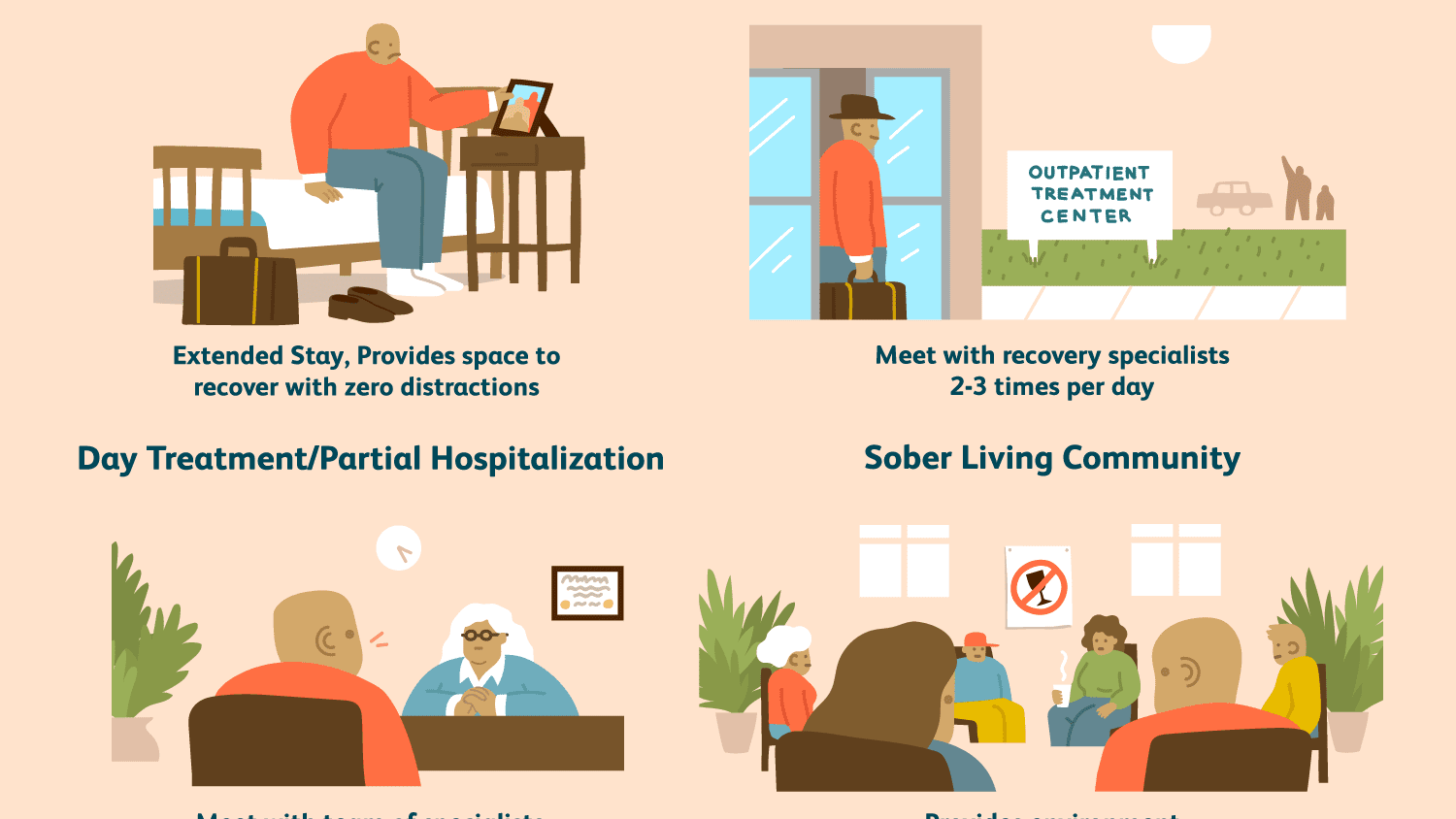
Inpatient Rehab
Inpatient rehabilitation facilities provide structured treatment programs that address all aspects of an individual’s addiction. Patients undergoing inpatient treatment dwell in a substance-free institution and get 24-hour medical and therapeutic support. Inpatient rehabs are an excellent alternative for persons who are battling chronic addiction or who have a co-occurring mental or behavioral condition.
Intensive Outpatient Programs
Outpatient rehabilitation centers are another type of comprehensive addiction treatment. These programs provide many of the same effective treatments and therapies as inpatient rehabilitation centers. Outpatient rehabs, on the other hand, allow patients to remain at home during the healing process. Patients may continue working and care for their families while attending weekly scheduled treatment sessions.
It’s critical to remember that outpatient therapy does not isolate patients from the outside world; as a result, patients are more likely to encounter triggers that threaten their recovery. Outpatient rehabs are therefore most suited for persons who have minor kinds of addiction and a committed, disciplined attitude to recovery. Outpatient treatment is also a good “step-down” program following inpatient treatment and is frequently integrated with sober living homes.
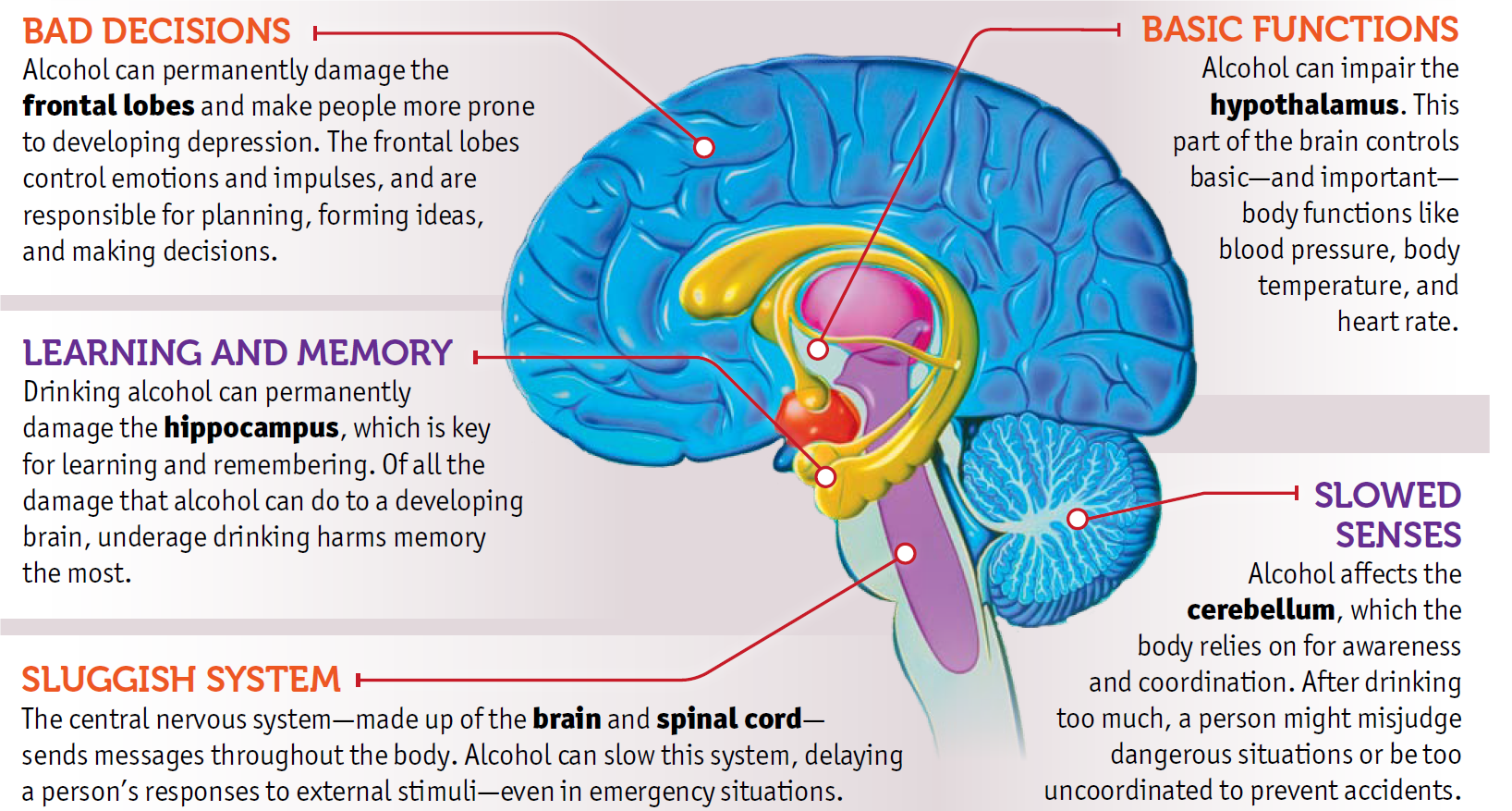
Drug and Alcohol Detox
Detoxification is a process that assists individuals in safely withdrawing from drugs or alcohol until the substances are no longer present in their system. It is frequently the first step in treating patients suffering from mild to severe addiction. Detoxing from certain drugs may require medicine to help alleviate the intensity of withdrawal symptoms. During detox, medications are frequently tapered down until the patient is no longer physiologically dependent on the addictive substance.
Sober Living Facilities
Sober living homes provide as a transitional housing option between an inpatient treatment center and reintegration into society. These are an excellent choice for individuals in recovery who require additional time to reinforce the lessons learnt in rehab. Sober living homes assist those in recovery in establishing new healthy habits while remaining in the safety of a structured environment.
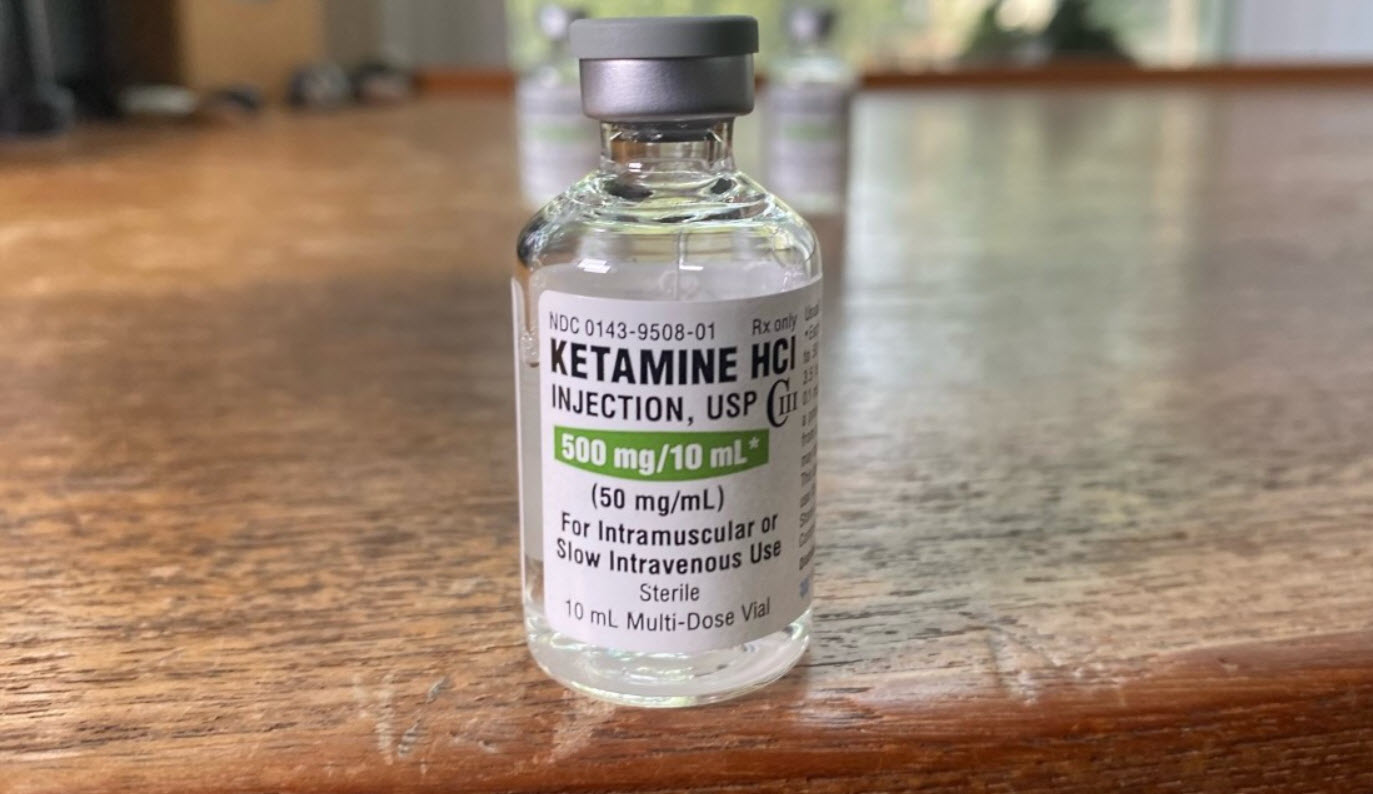
Addiction Treatment With Medical Assistance
Patients may be administered drugs to aid in the recovery process during detox and during therapy. These drugs are used to treat a number of conditions, including withdrawal symptoms, desire reduction, and co-occurring disorders. The most successful use of medications for addiction treatment is in conjunction with a comprehensive treatment program.
Interventions
An intervention is a meeting between loved ones and an addict that is frequently monitored by an intervention specialist. The purpose of an intervention is to assist loved ones in expressing their emotions constructively and to encourage an addict to enter a treatment program.
Faith Based – Christian Rehab
Certain individuals choose a more spiritual approach to healing. Faith-based rehabilitation institutions offer specific programs and facilities that are centered on the Christian faith. Within this type of rehabilitation program, persons in recovery can surround themselves with like-minded individuals who are seeking instruction from a higher power in order to remain strong throughout the journey ahead.